Osteoarthritis In Horses – Is There a New Option?
Clinical Connections – Spring 2023
Roger K.W. Smith, Professor of Equine Orthopaedics
The RVC Equine Referral Hospital had a world-first 20 years ago, when it cultured mesenchymal stem cells from the bone marrow of a horse suffering from an overstrain injury of its superficial digital flexor tendon. The cultured cells were implanted into the damaged tendon under ultrasound guidance.
While we felt cell therapy might offer significant benefits for the treatment of tendon injuries, based on laboratory work, we did not realise how much we didn’t know at the time. However, this spawned significant interest from around the world and the use of autologous mesenchymal stem cells became a commonly used treatment for both tendon and ligament injuries and osteoarthritis.
While the gradually accumulated clinical outcome data from tendon injuries was generally positive, the evidence for the effectiveness in osteoarthritis was more variable. Nevertheless, the use of stem cells became keenly adopted as an option for the treatment of inflammatory joint disease, especially in the USA.
However, the use of autologous stem cells carries limitations – they require obtaining the source material to culture the cells from, be it bone marrow or fat, and those procedures require technical expertise and an element of risk, particularly for aspiration of bone marrow from the sternum. Additionally, the second stage in the process requires culture of the cells in a VMD-licensed laboratory, which is costly. These have limited the use of stem cells.
One way around these limitations is to develop a stem cell product that is allogenic – i.e. cells derived from the same species but a different individual. This means multiple doses can be prepared from the same tissue of origin and supplied to the veterinary surgeon ‘off the shelf’, making their use much more convenient. However, because the cells are derived from a different individual, they can cause an allergic reaction when injected into the patient unless they are carefully characterised to reduce the risk.
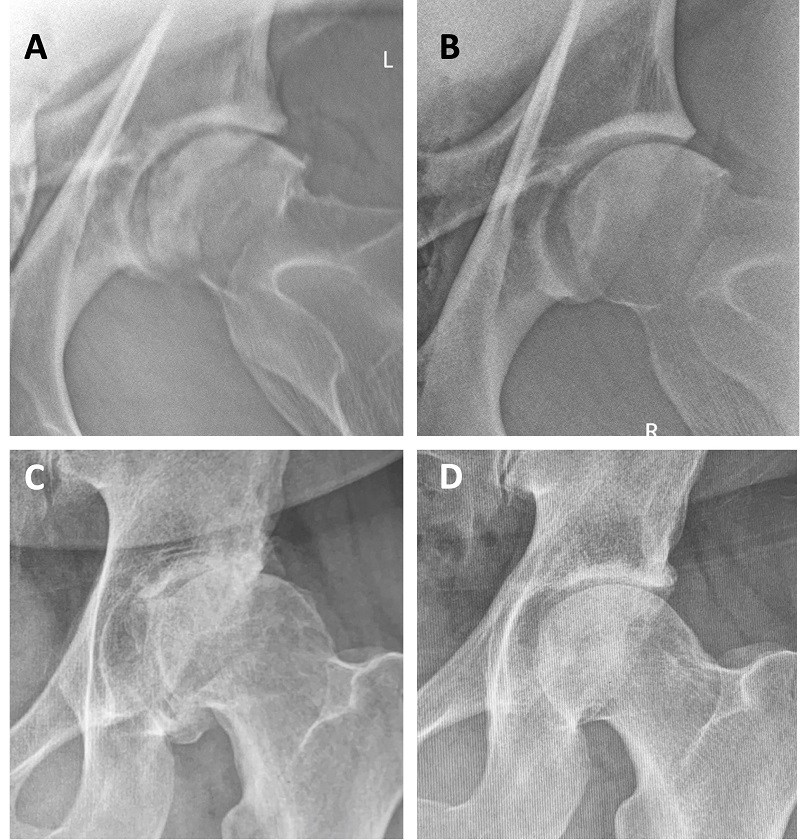
In 2019, Boehringer Ingelheim obtained a European-wide licence for an allogenic mesenchymal stem cell line, derived from blood and developed by a company in Belgium. This cell product has also had the cells ‘primed’ to make them more effective for the treatment of osteoarthritis (see figure 1).
RVC project
After this product was launched, Boehringer asked our Equine Referral Hospital to undertake a simple case-based ‘trial’. This was structured to allow us to assess any change in lameness after treatment by re-examinations at six and twelve weeks after treatment, using both the usual visual scoring and objective gait analysis, to minimise the subjectivity assessment. This system of lameness assessment is becoming mainstream in equine orthopaedics, and we have been using an in-house system, developed by Dr Thilo Pfau of the Structure and Motion Laboratory, for about ten years.
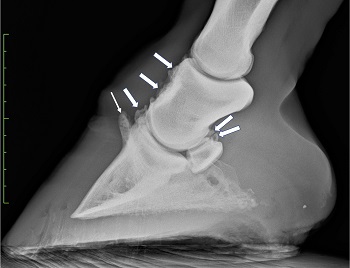
Recently, we concluded this trial and one of our students, Daniel Peterson, undertook assessment of the lameness data as part of a final year project, with interesting results. Visual and objective lameness assessment was recorded for fourteen patients (eg figure 2) at pre-treatment and at six and twelve weeks after treatment. Unfortunately, two patients could not complete further assessment – one due to concurrent laminitis and one as it was euthanised due to the severity of their OA.
Over the twelve-week study, visual lameness significantly decreased by a mean of 1.20 units (p=0.013). The evaluation of the objective gait analysis also showed a decrease in lameness, although this was not statistically significant – most likely because of the need to separate this analysis into forelimb and hindlimb cases, which reduced the statistical power of the study.
Interestingly, patients with a higher level of lameness on presentation responded to the treatment to a significantly greater magnitude (p= 0.0156). It was also observed that the decrease in lameness was greater at twelve weeks than six (p=0.0368), showing progressive improvement at a delay post-injection.
These results support the concept that stem cells can be beneficial for the treatment of one of the most common orthopaedic problems in horses, although it also suggests that the treatment does not always result in complete soundness. This may not be surprising when the cases selected were generally those more severely affected. This simple clinical study also illustrates the opportunities afforded by a university equine hospital, which provides research opportunities to our talented veterinary students – fostering skills appropriate for continuing clinical research throughout their careers.
