Dialysis and Therapeutic Plasma Exchange at RVC Small Animal Referrals – What are the options?
Clinical Connections – Spring 2019
Simon Cook, Lecturer in Emergency and Critical Care
The word dialysis may convey different things to different people, often conjuring images of human patients with chronic kidney failure, being hooked up to a dialysis machine several times a week until they are able to receive a transplant.
Fundamentally, dialysis means the removal of waste products and fluids from the body, but the dialysis machine we have at RVC Small Animal Referrals can be used in several different ways – in fact, we (currently) don’t use it at all for patients with chronic kidney disease.
There are three main ways in which we use our dialysis machine:
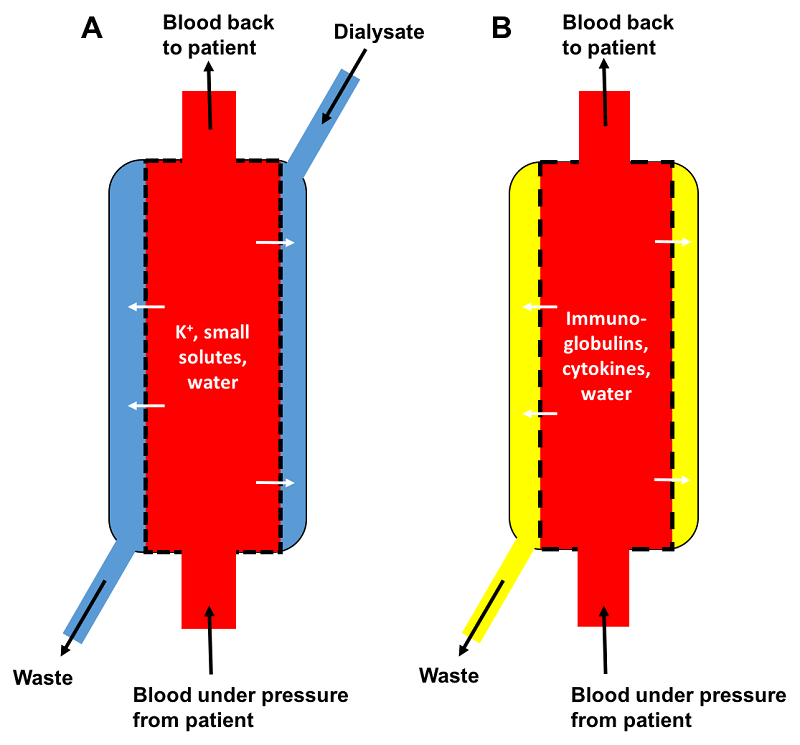
1. Removal of waste products (including potassium) and fluid that accumulates when the kidneys suddenly stop working, for any reason. These are patients with acute kidney injury (AKI). This process might be performed two or three times over the course of a week, giving the injured kidneys time to heal of their own accord. This is called haemodialysis.
2. Removal of toxins or overdosed drugs that are small molecules (e.g. ethanol, phenobarbital). This is also a form of haemodialysis but may only need to be performed once.
3. Removal of part of the patient’s plasma. This can be beneficial in patients with immune-mediated disease or in those with toxins or overdosed drugs that are large molecules or highly protein bound, such as non-steroidal anti-inflammatory drugs (NSAIDs). This is termed therapeutic plasma exchange (or plasmapheresis) – it involves removal of larger molecules, proteins including immunoglobulins, cytokines and fluid, while being replaced with donor plasma.
Each of these three scenarios are slightly different to dialysis typically offered to human patients with chronic kidney disease (CKD). Dialysis for CKD has been performed for dogs and cats in other countries but is a life-long treatment which we are not currently able to offer at the RVC. The main indication for dialysis at the RVC is therefore AKI.
There are a number of different toxins that we are able to remove with dialysis (see Box 1). However, one of the commonest toxicities that we see that causes kidney failure is ethylene glycol (EG) or antifreeze. To be effective with dialysis to treat EG toxicity, we need to start dialysis within a very narrow time window; <2-4 hours after ingestion. Unfortunately, this is rarely possible and once kidney failure has developed we no longer recommend dialysis for these patients as outcome is very poor.
You may also have seen that occasionally we have performed plasmapheresis in cases of cutaneous and renal glomerular vasculopathy (CRGV) or ‘Alabama rot’. We tend to advise this before the kidney damage has become severe, but please contact us if you have any questions.
The take home message would be to call us if you believe you have a patient who would benefit from dialysis or plasma exchange, or for advice. In particular, we are able to offer referral and advanced therapies for:
- Oligo-anuric acute kidney injury (AKI where urine output is declining or absent)
- Acute EG ingestion
- Overdoses: severe NSAID overdoses, phenobarbitone, azathioprine and others
- Immune-mediated disease that is refractory to early immunosuppression. e.g. immune-mediated haemolytic anaemia, immune-mediated thrombocytopenia, myasthenia gravis, polyradiculoneuritis
Please note that all of these procedures require placement of a large dialysis catheter into the jugular vein. Therefore, if you are considering referral for any form of ‘dialysis’ please avoid using the jugular veins where possible as poor venous access can make these treatments very difficult.
If you would like further information, please email for the attention of the RVC extracorporeal therapies team via QMHreception@rvc.ac.uk. Myself, Rosanne Jepson, Stefano Cortellini or Tom Greensmith would be happy to speak to you. For urgent enquiries please speak to the Emergency and Critical Care team.
